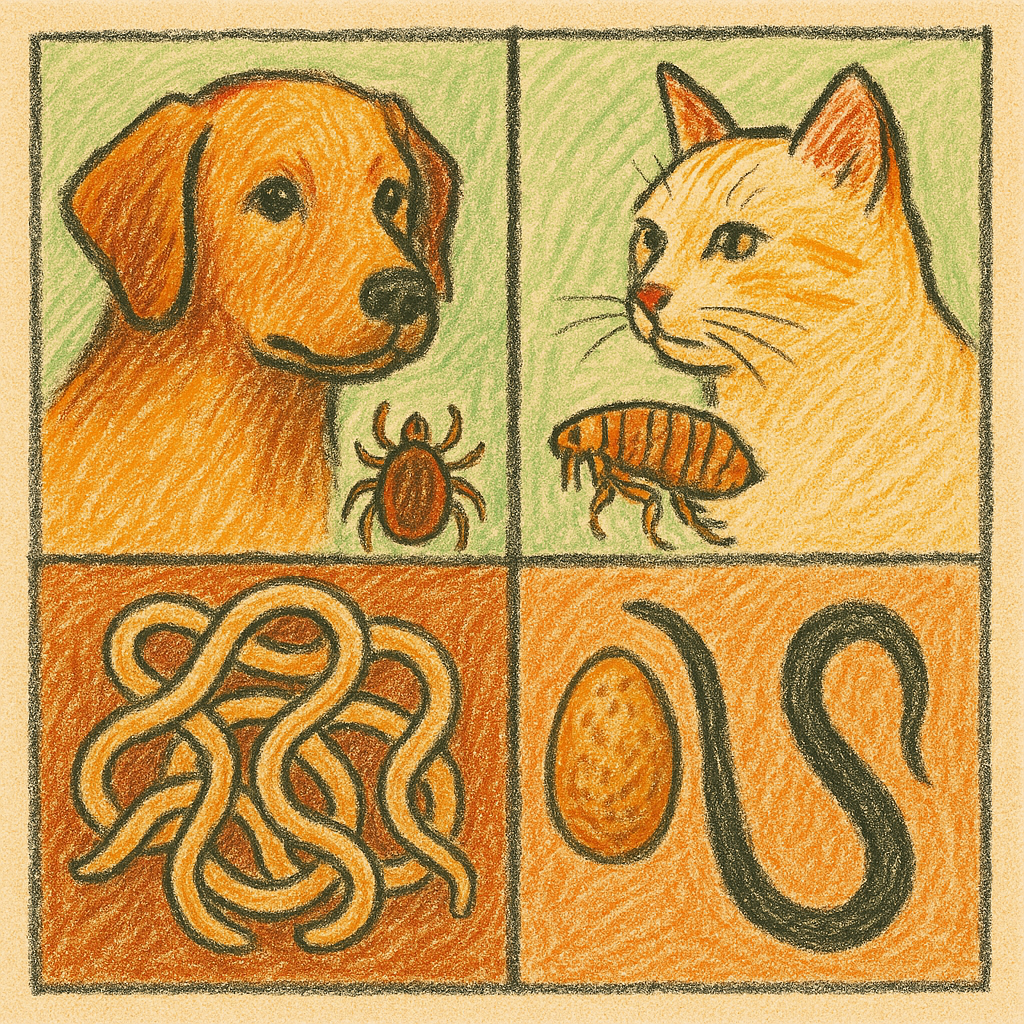
Comprehensive Guide to Parasites in Dogs and Cats: Fleas, Ticks, Worms & More
Companion animals host a broad array of ecto- and endoparasites that differ in biology, epidemiology and clinical importance. Effective control requires parasite-specific knowledge of life cycle stages, environmental reservoirs, transmission routes and the relative speed of development (which determines how rapidly infestations can escalate). The sections below dedicate a focused paragraph to each major parasite group, summarizing taxonomy, life cycle, ecology/habits, clinical consequences for animals and people, diagnostic pointers and best-practice eradication and prevention measures.
Fleas (primarily Ctenocephalides felis)
Adult cat fleas (most commonly Ctenocephalides felis, also found on dogs) have a holometabolous life cycle with four stages: egg → larva → pupa → adult. Development time is highly temperature- and humidity-dependent: under optimal indoor conditions the cycle can complete in about 2–8 weeks, whereas pupae can persist in the environment and delay emergence for months until cues (vibration, heat, CO₂) signal host presence. Because a large majority of a household population exists as eggs, larvae and pupae off the host, control must address both the animal and the environment.
Flea habits concentrate adults on host fur where females ingest blood and oviposit; eggs fall into resting sites (bedding, carpets, cracks). Larvae avoid light, feed on organic detritus and “flea dirt” (digested blood), then pupate in protected niches. Adult fleas are obligate hematophages and begin feeding within minutes of finding a host; however, many adult fleas will survive for days on animals while immature stages accumulate unseen in the environment.
Clinical impact ranges from localized pruritus to severe flea-allergy dermatitis (FAD) in hypersensitive animals; heavy infestations can cause significant blood loss and anaemia in puppies/kittens. Fleas also function as intermediate or mechanical vectors—classically transmitting Dipylidium caninum (tapeworm) when hosts ingest infected fleas and serving as potential mechanical carriers for bacterial pathogens.
Eradication requires integrated, simultaneous measures: fast-acting on-animal adulticides (oral or topical products that rapidly kill feeding fleas) combined with insect growth regulators (IGRs) or insect development inhibitors to prevent immature stages from maturing; rigorous environmental measures (frequent vacuuming with immediate disposal of bagged contents or emptied canister, laundering bedding at high temperatures, steam cleaning) and treatment of the premises when indicated. Treat all in-contact animals at once and maintain ongoing prophylaxis in at-risk animals to prevent reinfestation.
Ticks (hard ticks: Ixodes, Dermacentor, Rhipicephalus and others)
Hard ticks (Ixodidae) undergo four developmental stages—egg, larva, nymph, adult—and many medically relevant species are three-host ticks: each active stage feeds on a separate host then drops off to molt. The length of the complete life cycle varies from a single year in warm climates to several years in temperate or high-elevation regions, with diapause patterns determined by species and environment. Questing behavior (waiting on vegetation or in leaf litter) brings ticks into contact with passing hosts; species have ecological preferences (e.g., Ixodes in woodland/leaf litter; Rhipicephalus sanguineus, the brown dog tick, survives in kennels and peridomestic structures).
Ticks attach firmly and feed slowly over hours to days; this extended attachment period enables transmission of a variety of bacterial, protozoal and viral pathogens (regional examples include Borrelia spp. (Lyme), Anaplasma, Ehrlichia, Babesia, and spotted-fever group Rickettsia), and certain species secrete neurotoxins that cause tick paralysis. Local skin damage, secondary infection at the bite site and, in heavy infestations, anaemia can occur.
Control emphasizes regular inspection and prompt mechanical removal using fine-tipped forceps or specialized tick tools (grasp close to the mouthparts and pull steadily; avoid crushing the tick), plus the routine use of licensed acaricidal or systemic tick-control products appropriate for the host species and regional tick fauna. Habitat modification (short grass, removal of leaf litter, barrier zones) and treating kennels or resting sites for peridomestic species reduce environmental pressure. In endemic areas, testing and veterinary screening for tick-borne pathogens is indicated when clinical signs arise.
Mite groups differ sharply in biology: Sarcoptes scabiei is an obligate burrowing mite whose entire approximately 2–3 week life cycle occurs on the host epidermis (eggs → larvae → nymphs → adults) and transmits readily by direct contact; Demodex species are commensal follicular mites (normal at low densities) whose overgrowth (localized or generalized demodicosis) reflects immunologic or genetic predisposition; Otodectes cynotis completes its life cycle in the ear canal and adjacent skin and spreads by close contact.
Behaviorally, sarcoptic mites burrow in the superficial epidermis and provoke intense pruritus, papular dermatitis and crusting lesions; demodex overgrowth causes folliculitis, scaling and alopecia and is commonly complicated by secondary bacterial pyoderma; otodectes produce severe otitis externa with characteristic dark ceruminous debris. Humans exposed to canine sarcoptic mites may develop transient pruritic lesions, but human infestation is typically self-limiting because mites do not reproduce well on people.
Diagnosis combines clinical pattern recognition with parasitologic demonstration: superficial skin scrapings or acetate tape preparations may reveal sarcoptic mites (but false negatives are common), deep scrapings or trichograms/skin biopsies can demonstrate Demodex, and otoscopy plus ear cytology identifies ear mites. Management includes host-directed acaricides (oral systemic isoxazoline compounds, topical selamectin or spot-ons, amitraz dips for specifically labeled canine use, or macrocyclic lactones where indicated), repeated treatments to cover the mite life cycle, treating all in-contact animals for contagious forms, and addressing underlying predisposing disease for demodicosis (endocrinopathies, immunosuppression). Environmental decontamination (bedding laundering, isolation of newly acquired animals) complements therapy for contagious mites.
Intestinal nematodes — ascarids (Toxocara canis, T. cati) and hookworms (Ancylostoma spp.)
Ascarids and hookworms have direct or complex transmission routes and environmentally resistant stages that drive persistence. Toxocara canis and T. cati produce thick-shelled eggs that require days to weeks in soil to embryonate to the infective stage; T. canis commonly transmits vertically (transplacental) and transmammarily to puppies, while ingestion of embryonated eggs or paratenic hosts also transmits infection. Hookworm larvae (e.g., Ancylostoma spp.) develop in moist soil and infect hosts either by ingestion or percutaneous larval penetration; some species also transmit via transmammary routes. These lifecycle characteristics create persistent environmental exposure risks in contaminated areas.
Clinical disease in animals ranges from subclinical intestinal carriage to severe enteritis, poor growth, weight loss and iron-deficiency anaemia in heavy burdens — puppies and kittens are especially vulnerable. Zoonotic consequences are significant: ingestion of embryonated Toxocara eggs can cause visceral or ocular larva migrans in humans; skin-penetrating hookworm larvae (certain Ancylostoma spp.) cause cutaneous larva migrans.
Diagnosis relies on fecal flotation (centrifugal flotation increases sensitivity) and periodic surveillance; migrating larvae or prepatent infections can evade detection, so clinical context and age justify empirical deworming in young animals. Control is twofold: strategic anthelmintic protocols (serial deworming of neonates/juveniles with agents effective against ascarids and hookworms — pyrantel, fenbendazole, others — transitioning to risk-based testing and treatment in adults) plus environmental sanitation (prompt feces removal, preventing access to contaminated soil or scavenging) and owner education to protect human health.
Tapeworms (Dipylidium caninum and taeniids)
Tapeworms are cestodes that require intermediate hosts. Dipylidium caninum uses fleas (and occasionally lice) as obligate intermediate hosts: flea larvae ingest egg packets, the tapeworm metacestode matures within the flea, and the definitive host becomes infected by ingesting an infected flea during grooming. Other taeniid tapeworms require ingestion of infected intermediate hosts (rodents, rabbits) and have different public-health implications (some species are zoonotic).
Clinical effects are usually mild: intermittent anal irritation, visible rice-like proglottids in feces or perianal hair and occasional nonspecific gastrointestinal signs. Diagnosis typically relies on observation of proglottids or fecal flotation (sensitivity is limited for segmented tapeworms). Effective eradication requires both praziquantel or epsiprantel treatment to remove adult cestodes and concurrent interruption of the vector or intermediate host cycle — chiefly rigorous flea control to prevent D. caninum reinfection and preventing predation to reduce exposure to taeniid metacestodes.
Heartworm (Dirofilaria immitis)
Heartworm is a mosquito-borne filarial nematode: microfilariae circulate in the blood of an infected definitive host, are ingested by a mosquito and develop in the vector to an infective L3 stage (development is temperature-dependent), then are transmitted to a new host during subsequent mosquito blood meals. In the mammalian host larvae migrate and mature over months into adult worms that occupy the pulmonary arteries and right heart, producing a progressive cardiopulmonary syndrome in dogs; cats are susceptible but typically develop lower worm burdens with different clinical manifestations, including acute respiratory signs or sudden death.
Because established adult infections are difficult and potentially hazardous to treat (adulticidal protocols require staged, monitored therapy to reduce thromboembolic risk), prevention dominates control strategy. Monthly macrocyclic-lactone chemoprophylaxis (ivermectin, moxidectin, milbemycin, selamectin formulations) reliably kills early larval stages and is the standard of care in endemic regions. Annual testing (antigen and microfilariae testing in dogs) before and during prophylactic programs is recommended by major parasitology groups, and mosquito-exposure mitigation (screens, repellents and habitat management) complements chemoprophylaxis.
Protozoa — Giardia and coccidia (Isospora, Cystoisospora)
Protozoal intestinal parasites have direct fecal-oral cycles with environmentally resistant infectious stages (cysts or oocysts). Giardia alternates between fragile trophozoites in the intestine and robust cysts in feces; cysts can survive for days to weeks in moist cool environments and are infectious on ingestion. Canine and feline coccidia (e.g., Cystoisospora spp.) produce oocysts that sporulate in the environment and transmit by ingestion.
Clinically these infections commonly cause diarrhea (sometimes severe in neonates or immunocompromised animals), weight loss and malabsorption. Diagnostic approaches include antigen tests and fecal flotation/concentration for cysts and oocysts; PCR can be used for genotyping in epidemiologic or zoonotic investigations. Treatment and eradication depend on accurate diagnosis: metronidazole or fenbendazole regimens for giardiasis in many protocols, and sulfonamides (e.g., sulfadimethoxine) for clinical coccidiosis, combined with environmental sanitation (rapid feces removal, drying/heat disinfection, steam cleaning) to remove infectious stages and prevent reinfection.
Lice (Mallophaga — chewing lice; Anoplura — sucking lice)
Lice are permanent, host-specific ectoparasites with direct life cycles (egg/nit → nymph → adult) that complete entirely on the host. Heavy infestations arise in animals with poor grooming, overcrowding or compromised health. Chewing lice feed on skin debris and cause pruritus and scaling; sucking lice ingest blood and can induce anaemia in severe cases. Lice survive poorly off the host, so transmission is primarily by close contact. Diagnosis is by visual detection, nit identification or close inspection with a fine comb; eradication uses topical insecticides labeled for lice and treating all in-contact animals plus environmental cleaning of bedding and grooming equipment.
Diagnostic & control algorithm (practical, vet-oriented)
- Routine screening: fecal flotation (centrifugal) at least twice yearly in adults and more frequently in young animals; annual heartworm antigen and microfilaria testing in dogs; tick-borne pathogen testing as indicated by region and exposure.
- Rule out competing causes: perform skin scrapings, ear cytology, flea combing and fungal/bacterial cultures as indicated by signs.
- Treat the host and the environment: for fleas and tapeworms treat both animal (adulticides + anthelmintics) and environment (vacuum, launder, insect growth regulators); for ticks focus on prompt removal and ongoing acaricide prophylaxis; for intestinal helminths use appropriately selected anthelmintics and repeat fecal monitoring; for heartworm use prevention and, if infected, follow staged adulticidal protocols under veterinary supervision.
- Public-health measures: deworm puppies/kittens per schedule, remove feces promptly, discourage pica and geophagia, protect children from contaminated soil, and counsel owners on hand hygiene to reduce zoonotic risk from Toxocara and cutaneous larval migrans.
Practical eradication checklist (owner-facing, actionable)
- Fleas: start licensed on-animal product (fast systemic adulticide + IGR), vacuum daily for first 2–4 weeks, wash bedding weekly, treat all pets and repeat environmental measures until no new adults observed.
- Ticks: inspect daily in high-risk months, remove attached ticks promptly with a tick tool, use year-round tick control products where ticks are endemic, modify yard to reduce habitat.
- Intestinal worms: follow neonatal/juvenile deworming schedules, perform routine fecals, prevent hunting/scavenging, educate on zoonotic risks.
- Heartworm: administer monthly macrocyclic lactone prophylaxis as recommended; test annually.
GreenFreshPets.com focuses on minimally processed, dehydrated pet nutrition built from identifiable whole-food ingredients. Because properly dehydrated diets are produced under controlled time–temperature conditions and reduced water activity, they create an inhospitable environment for many parasite stages that can survive in poorly handled raw foods. This combination of hygienic processing and preserved nutrient integrity offers a practical way to reduce food-borne parasite risk while supporting consistent, clean nutrition for dogs and cats.


